|
August 2020 NEW THERAPY TARGETS BREAST CANCER METASTASES IN BRAINFeaturing: Maciej Lesniak, MD
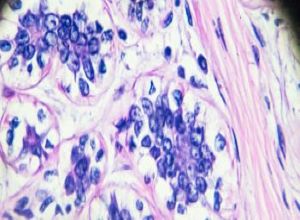
Combination therapy reduces tumor size, dramatically improves survival in mice When breast cancer spreads to the brain, the prognosis is grim. Patients only have about six months to live. Women with HER2-positive breast cancer tend to develop brain metastases in up to 55% of cases. Chemotherapy drugs targeting breast cancer cells in the brain aren’t effective because they can’t cross the blood-brain-barrier. But a new combination therapy targeting breast cancer tumors in the brain dramatically decreased tumor size and increased survival in a study with mice, reports a new Northwestern Medicine study published in Science Translational Medicine. An estimated 75% of mice that had brain metastases from breast cancer were cured and cancer-free after the therapy. “The new combination therapy we identified can cross the blood-brain barrier,” said lead study author Maciej Lesniak, MD, chair and Michael J. Marchese Professor of Neurological Surgery and chair of neurosurgery at Northwestern Memorial Hospital. “The therapy also targets brain metastases and significantly improves survival.” The two drugs are tubulin inhibitor, vinorelbine, approved by the U.S. Food and Drug Administration (FDA) and available in clinics, and bromodomain inhibitor, I-BET-762, FDA approved for clinical trials. The bromodomain inhibitor increased βIII-tubulin, a protein found in cancer cells that metastasize to the brain. Overexpression of βIII-tubulin sensitized cancer cells to be killed by vinorelbine. “The findings of our work set the stage for a clinical trial, whereby patients with breast cancer brain metastases can be treated with the combination of these two drugs,” said Lesniak, who is also leader of the Neuro-Oncology Program at the Robert H. Lurie Comprehensive Cancer Center of Northwestern University. “This will offer patients with breast cancer brain metastases who have been systematically excluded from clinical trials the chance to benefit from a new therapeutic regimen that has been proven to be strongly effective in experimental settings.” Breast cancer spreads to other organs like the brain, lung and bone. The metastasis of breast cancer to the brain is a terminal disease and the deadliest complication. There is a lack of targeted therapies for breast cancer brain metastases, said first study author Deepak Kanojia, PhD, research associate in neurological surgery. “Patients with brain metastases are often excluded from clinical trials due to their poor outcomes and dismal survival,” Kanojia said. “Regular systemic therapies, like Herceptin, do not cross the blood-brain barrier efficiently, and offer no benefit in brain metastases,” he said. How the study worked Scientists developed a mouse model that can grow multiple brain metastases to simulate what happens in human patients. They injected tumor cells in the intracarotid artery, resulting in the formation of multiple brain tumors. After the tumors grew, scientists treated the mice with the combination therapy. Final results revealed that 75% of the mice that were treated with the combination were cured and cancer-free. Other Northwestern authors include co-first author Wojciech Panek, DVM, Craig Horbinski, MD, PhD, director of neuropathology and professor in the Department of Pathology, Irina Balyasnikova, PhD, associate professor of Neurological Surgery, and Atique Ahmed, PhD, assistant professor of Neurological Surgery, Jason Miska, PhD, research assistant professor of Neurological Surgery, Alex Cordero-Casanovas, PhD, Jawad Fares, MD, Solomiia Savchuk, Krishan Kumar, PhD, Ting Xiao, MS, Katarzyna Pituch, PhD, Peng Zhang, PhD, and Kwok-Ling Kam, MBBS. Horbinski, Balyasnikova, Ahmed and Miska are all members of the Lurie Cancer Center. The research was supported by grants R35CA197725, R01NS093903, P50CA221747, R01NS87990, R01NS106379 01A1, 1R01NS096376-01A1, 5R21CA220625 and R01NS102669 from the National Institutes of Health. This article was originally published in the Feinberg School of Medicine News Center on August 27, 2020. |
Maciej Lesniak, MD, chair and Michael J. Marchese Professor of Neurological Surgery and chair of neurosurgery at Northwestern Memorial Hospital, and lead author of the study.
Refer a PatientNorthwestern Medicine welcomes the opportunity to partner with you in caring for your patients.
|
You May Also Like
|
October 2020 |