|
August 2022 INVESTIGATING THE UTILITY OF POLYGENIC RISK SCORES FOR CHDFeaturing: Sadiya Khan, MD, MSc
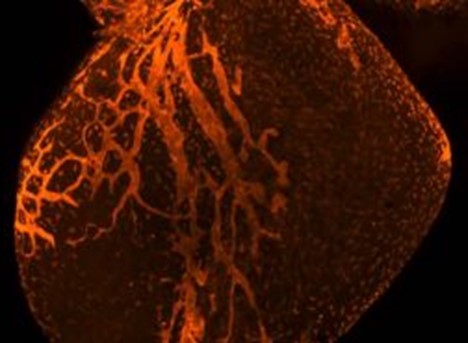
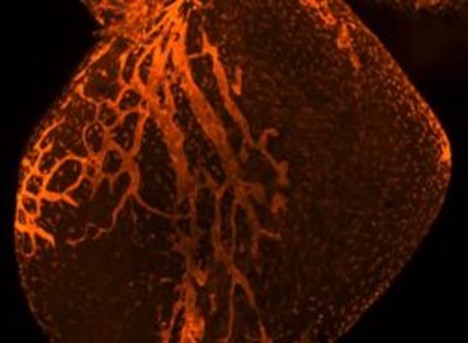
A polygenic risk score for coronary heart disease (CHD) — which aggregates the risk associated with many commonly occurring genetic variants or an individual’s inherited risk — demonstrated minimal clinical utility in improving long-term risk prediction of CHD when combined with routine patient clinical data, according to findings published in Circulation. “Since the completion of the human genome map, there has been a significant push for clinical integration of precision medicine approaches into patient care, but it remains uncertain whether integrating genetic risk based on a polygenic risk score for coronary heart disease improves our ability to identify who is at risk. We wanted to address this important knowledge gap, particularly among young adults,” said Sadiya Khan, ’09 MD, ’14 MSc, ’10, ’12 GME, assistant professor of Medicine in the Division of Cardiology, of Preventive Medicine in the Division of Epidemiology and lead author of the study. Life expectancy in the U.S. has continuously declined since 2014, which has been partially attributed to an increase in cardiovascular disease mortality among young and middle-aged adults. Those who experience premature atherosclerotic cardiovascular disease, such as CHD, may experience modifiable risk factors that provide opportunities for early prevention and long-term clinical benefit. This has led to an increased focus on early identification and prevention of CHD in both young and middle-aged adults in the U.S. over the last decade. Advances in genomic data analysis and availability, such as with polygenic risk scores, have generated the potential for precision medicine approaches for many diseases. While there is potential to measure risk early in adulthood, the accuracy and clinical utility of polygenic risk scores in predicting long-term risk of CHD had not yet been explored. In the current study, investigators analyzed data from more than 9,700 white adults between the ages 20 to 59 years who were enrolled in two population-based cohorts — the Framingham Offspring Study and the Atherosclerosis Risk in Communities study. The team aimed to determine whether a PRS-based approach was more effective than a 30-year risk model using traditional risk factor levels such as weight, blood pressure and cholesterol. In young adults, the investigators identified a small, statistical change in in model discrimination for CHD when the polygenic risk score was added to the traditional risk factor score. However, the overall change was determined clinically insignificant. In midlife adults, the investigators observed no change. “Among young or early-midlife adults predicted to be at low risk on the basis of traditional risk factors, a high polygenic risk score did not significantly increase the risk of coronary heart disease,” according to the authors. The findings underscore that traditional risk factors, which are routinely assessed during a patient’s primary care appointment, are effective and reliable in predicting 30-year risk of CHD and identify young adults who may benefit from more intensive prevention strategies. Philip Greenland, MD, Harry W. Dingman Professor of Cardiology and a member of the Robert H. Lurie Comprehensive Cancer Center of Northwestern University, was a co-author of the study. This work is supported by grants from the National Institutes of Health (P30AG059988, R01HL159250 and U01HL160279) and the American Heart Association grant 19TPA34890060. This article was originally published in the Feinberg School of Medicine News Center on August 30, 2022. |
Sadiya Khan, MD, MSc, 09 MD, ’14 MSc, ’10, ’12 GME, assistant professor of Medicine in the Division of Cardiology and of Preventive Medicine in the Division of Epidemiology, was lead author of the study published in Circulation.
Refer a PatientNorthwestern Medicine welcomes the opportunity to collaborate with you in caring for your patients.
|
You May Also Like
|
December 2021 |
December 2021 |
November 2021 |